PPMI integration
Baseline-first harmonization of 4,775 patients across 388 features covering MDS-UPDRS, UPSIT, REM sleep behavior disorder, biospecimens, and genetics.
We continually evaluate our pipelines across imaging, diffusion, wearables, and clinician-facing deployment. This page summarizes quantitative readouts, cohort coverage, and the evidence trail that underpins Progressive AI.
Baseline-first harmonization of 4,775 patients across 388 features covering MDS-UPDRS, UPSIT, REM sleep behavior disorder, biospecimens, and genetics.
2,958 participants inform genetic risk analyses and mechanism inference, highlighting the 1.89× elevated risk among G2019S carriers.
84 idiopathic Parkinson’s participants with synchronized CSFSAA labels, IMU-derived gait metrics, and comprehensive cognitive batteries.
ActionIntel and Free Motion prototypes evaluated with neurologists in weekly design reviews to pressure-test usability and interpretability.
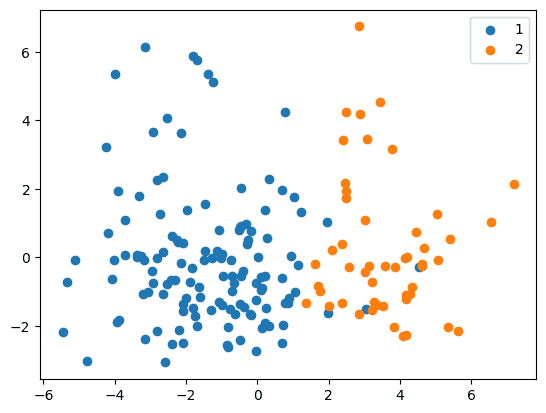
Automated SegFormer-based segmentation combined with DaT-SPECT features enables high-fidelity CSFSAA discrimination. Results below reflect cross-validated models trained on region-wise volumetrics and SBR-derived statistics.
| Method | F1-score | ROC-AUC |
|---|---|---|
| Nearest Neighbors | 0.960 | 0.900 |
| Random Forest | 0.950 | 0.858 |
| Neural Network | 0.950 | 0.843 |
| Gaussian Process | 0.944 | 0.837 |
| Naive Bayes | 0.935 | 0.907 |
Imaging alone yields AUC 0.70 ± 0.08; combining imaging with clinical and biologic features raises AUC to 0.93 ± 0.04.
Histogram Gradient Boosting models trained on PPMI gait assessments quantify the contribution of each modality toward predicting CSFSAA status.
| Feature Group | Mean AUC ± SD |
|---|---|
| Gait & Arm Swing | 0.58 ± 0.16 |
| Demographics | 0.81 ± 0.14 |
| Clinical | 0.92 ± 0.07 |
| All Modalities | 0.93 ± 0.07 |
SHAP analysis surfaces HVLT retention, Epworth Sleepiness Scale, and right-arm jerk amplitude as leading contributors.
We are expanding evaluation to prospective, multi-site cohorts with emphasis on drift audits, fairness reporting, and regulatory documentation. Outcomes will be updated quarterly as we release new validation notes and open-source assets.